Understanding the Essentials of Biomarker Analysis: An In-depth Exploration
In the ever-evolving field of medical research, biomarker analysis plays a crucial role in understanding diseases, identifying therapeutic targets, and monitoring treatment outcomes. This article aims to provide an in-depth exploration of the essentials of biomarker analysis, shedding light on its definitions, significance, scientific underpinnings, challenges, and future perspectives. By delving into this vast scientific domain, the hope is to unravel the intricate world of biomarkers and their potential impact on healthcare.
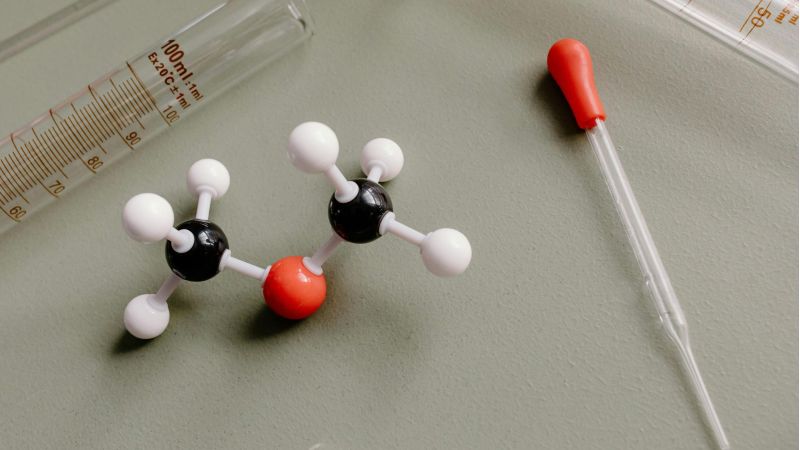
Defining Biomarkers: A Brief Overview
ALT TXT IMG: A text inside a heart-shaped card promoting a healthy lifestyle
To comprehend the intricacies of biomarker analysis, it is imperative to first define what biomarkers are. Simply put, biomarkers are measurable and quantifiable indicators that objectively reflect biological processes, pathological states, or responses to therapeutic interventions. They can manifest as molecules, genes, proteins, cells, or even imaging features, providing valuable insights into individual health, disease progression, and treatment efficacy.
By analyzing biomarkers, researchers can gain a deeper understanding of diseases at a molecular level, enabling more precise diagnosis, prognosis, and personalized treatment strategies. Biomarkers have become an integral part of medical research, revolutionizing the way diseases are diagnosed, monitored, and treated.
The Role and Importance of Biomarkers in Medical Research
“It’s more important to understand the imbalances in your body’s basic systems and restore balance, rather than name the disease and match the pill to the ill.”
–Mark Hyman, M.D.
Biomarkers play a pivotal role in medical research, contributing to advancements in diagnosis, risk stratification, and therapeutic interventions. As surrogate endpoints, biomarkers can help predict treatment response, efficacy, and safety, thus expediting drug development pipelines and reducing costs associated with clinical trials.1
Moreover, biomarkers empower early disease detection and aid in the identification of high-risk individuals, enabling targeted interventions for preventative measures. Their non-invasive nature also means that biomarkers can be used for longitudinal monitoring, tracking disease progression, or treatment response in real-time.
For instance, in the field of cancer research, biomarkers have revolutionized the way tumors are diagnosed and treated. By analyzing specific biomarkers present in tumor cells, oncologists can determine the most effective treatment options for individual patients, leading to improved outcomes and reduced side effects.
Furthermore, biomarkers have also played a crucial role in the development of precision medicine2, where treatments are tailored to an individual’s unique genetic makeup and biomarker profile. This approach has shown promising results in various diseases, such as cardiovascular disorders, neurological conditions, and autoimmune disorders.
Different Types of Biomarkers and Their Specific Uses
Biomarkers encompass various categories, each serving a distinct purpose in the realm of medical research. Some common types of biomarkers include:
- Diagnostic Biomarkers: These biomarkers aid in identifying the presence or absence of a disease or condition. They provide critical information for accurate diagnosis and subsequent treatment planning.
- Prognostic Biomarkers: Prognostic biomarkers offer insights into an individual’s disease outcome. They can help predict the likelihood of disease progression, recurrence, or response to treatment.
- Predictive Biomarkers: Predictive biomarkers assess the likelihood of response to a specific treatment or therapy. They assist in tailoring interventions and optimizing patient management.
- Surrogate Endpoints: Surrogate endpoints act as proxy measurements, standing in for clinical outcomes that are more difficult or time-consuming to assess. They serve as reliable indicators of treatment benefit or harm.
By leveraging these different types of biomarkers, researchers can gain a comprehensive understanding of diseases and develop targeted approaches for patient care.
For example, in cardiovascular research, diagnostic biomarkers such as troponin levels are used to identify the presence of a heart attack. Prognostic biomarkers, such as brain natriuretic peptide (BNP), can help predict the risk of heart failure in patients with cardiovascular disease. Predictive biomarkers, like genetic variants associated with drug metabolism, can guide clinicians in selecting the most effective medication for an individual patient.
Surrogate endpoints, such as blood pressure or cholesterol levels, are often used in clinical trials to evaluate the effectiveness of new drugs or interventions without waiting for long-term clinical outcomes.
Overall, biomarkers have transformed the medical research landscape, enabling more precise diagnoses, personalized treatments, and improved patient outcomes. As technology advances and our understanding of biomarkers deepens, the potential for further advancements in healthcare is vast.
ALT TXT IMG: Human skeleton with a visual representation of DNA, showcasing the connection between genetics and the skeletal structure
The Science Behind Biomarker Analysis
At the core of biomarker analysis lies the meticulous process of identifying and analyzing these intricate indicators. This section explores the scientific methodologies and technological advancements that facilitate biomarker research and enable its translation into clinical practice.
Biomarkers are biological molecules or genetic signatures that can be measured and evaluated to indicate normal biological processes, pathogenic processes, or pharmacological responses to a therapeutic intervention. They play a crucial role in disease diagnosis, prognosis, and treatment monitoring.
The Process of Identifying and Analyzing Biomarkers
Biomarker discovery is a multidisciplinary endeavor involving various stages and methodologies. Initially, researchers identify potential biomarkers by collecting biospecimens from individuals with and without the disease of interest. Comparative analyses, such as genomic or proteomic profiling, help identify molecules or genetic signatures that differentiate diseased and healthy states.
Once potential biomarkers are identified, validation studies are conducted to assess their diagnostic, prognostic, or predictive performance across diverse patient populations. These studies involve rigorous statistical analyses and independent validation cohorts to ensure the reliability and generalizability of the identified biomarkers.
Technological Advances in Biomarker Analysis
Rapid advancements in technology have revolutionized biomarker analysis, expanding the possibilities for precision medicine and personalized healthcare. High-throughput sequencing technologies enable comprehensive genomic profiling, empowering the identification of genetic biomarkers and molecular subtypes of diseases.
Furthermore, imaging modalities, such as positron emission tomography (PET) and magnetic resonance imaging (MRI), provide valuable spatial and functional information, facilitating the development of imaging biomarkers for disease characterization and monitoring.
Additionally, novel analytical techniques, such as mass spectrometry and next-generation sequencing, have enhanced the sensitivity, specificity, and throughput of biomarker analysis, opening up new avenues for discovery and validation.
These technological advances continue to shape the field of biomarker analysis, propelling research forward and revolutionizing patient care. Moreover, the integration of artificial intelligence (AI)3 and machine learning algorithms has further accelerated biomarker analysis. AI algorithms can process large volumes of data, identify patterns, and make predictions, aiding in identifying and interpreting complex biomarker profiles.
Furthermore, the development of microfluidic devices and lab-on-a-chip technologies has streamlined biomarker analysis by enabling miniaturization, automation, and high-throughput screening. These devices allow for the analysis of multiple biomarkers simultaneously, reducing cost, time, and sample requirements.
Moreover, the emerging metabolomics field has expanded the biomarker analysis scope. Metabolomics involves the comprehensive analysis of small molecules, known as metabolites, present in biological samples. By profiling the metabolome, researchers can gain insights into cellular processes, identify disease-specific metabolic alterations, and discover novel biomarkers.
In conclusion, biomarker analysis is a complex and dynamic field that relies on scientific methodologies and technological advancements. The identification and analysis of biomarkers involve a multi-step process, from discovery to validation, and require the integration of various analytical techniques. Technological advances, such as high-throughput sequencing, imaging modalities, and novel analytical techniques, have revolutionized biomarker analysis, enabling precision medicine and personalized healthcare. The integration of AI, microfluidic devices, and metabolomics further enhances biomarker analysis, propelling research forward and transforming patient care.
The Challenges in Biomarker Analysis
While biomarker analysis holds immense promise, it also poses significant challenges that must be addressed to ensure its successful translation into clinical practice. This section highlights some key issues researchers and healthcare professionals face when dealing with biomarker analysis.
Biomarker analysis is a complex process that involves the identification, validation, and verification of specific molecules or characteristics that can indicate the presence or progression of a disease. It is crucial in disease diagnosis, prognosis, and treatment selection. However, several challenges need to be overcome to harness the full potential of biomarkers in improving patient outcomes.
Issues in Biomarker Validation and Verification
Robust validation and verification of biomarkers are essential for their successful translation into clinical practice. Insufficient reproducibility and lack of standardization can hinder biomarker development and limit their utility. To overcome these challenges, rigorous study design, appropriate statistical methods, and independent validation in diverse patient populations are crucial.
Validation of biomarkers involves assessing their accuracy, precision, and reliability. It requires extensive testing in different cohorts to ensure that the biomarker consistently provides meaningful and reliable results. Verification, on the other hand, focuses on confirming the clinical utility of the biomarker and its ability to improve patient outcomes when used in real-world settings.
Standardization is another critical aspect of biomarker analysis. Without standardized protocols and guidelines, different laboratories may use different methods, leading to inconsistent results. This lack of standardization not only hampers the comparison of results across studies but also limits the integration of biomarkers into clinical practice.
Ethical Considerations in Biomarker Analysis
As biomarker analysis becomes more pervasive, ethical considerations also come into play. The use of biospecimens, the potential invasiveness of certain biomarker analyses, and the privacy concerns associated with data sharing necessitate careful ethical deliberation and informed consent procedures.
Researchers must ensure that the collection and use of biospecimens for biomarker analysis are conducted ethically and with the utmost respect for patient autonomy and privacy. Informed consent procedures should be implemented to ensure that individuals understand the purpose, risks, and benefits of participating in biomarker studies.
Furthermore, the commercialization of biomarker-based diagnostics and therapies raises concerns about equitable access to these advancements. It is essential to strike a balance between promoting innovation and ensuring that biomarker-based technologies are accessible to all individuals, regardless of their socioeconomic status or geographic location.
By addressing these ethical considerations, researchers and healthcare professionals can build public trust and confidence in biomarker analysis, facilitating its integration into routine clinical practice.
Future Perspectives on Biomarker Analysis
Looking ahead, the field of biomarker analysis holds immense potential for revolutionizing healthcare and personalized medicine. Exciting developments and emerging trends are shaping the future of biomarker research and its clinical applications.
In recent years, there has been a surge in interest and investment in precision medicine, which aims to tailor medical treatments to individual patients based on their unique genetic makeup, lifestyle, and environmental factors. This approach has paved the way for advancements in biomarker research as scientists strive to identify specific molecular indicators that can predict disease susceptibility, treatment response, and prognosis.
One of the emerging trends in biomarker research is the integration of multi-omic datasets. By combining information from genomics, proteomics, metabolomics, and other -omics disciplines, researchers can gain a more comprehensive understanding of disease mechanisms and identify novel biomarkers with higher accuracy and specificity. This holistic approach has the potential to revolutionize the way diseases are diagnosed, monitored, and treated.
Another exciting development is the application of artificial intelligence (AI) and big data analytics in biomarker analysis. AI algorithms can analyze vast amounts of patient data, including clinical records, imaging data, and molecular profiles, to identify patterns and correlations that may not be apparent to human researchers. This data-driven approach can accelerate biomarker discovery, facilitate patient stratification, and enable more precise treatment optimization.
Emerging Trends in Biomarker Research
Advancements in precision medicine, artificial intelligence, and big data analytics are revolutionizing biomarker research. Integrating multi-omic datasets, harnessing machine learning algorithms, and leveraging deep learning approaches offer unprecedented opportunities for biomarker discovery, patient stratification, and treatment optimization.
Furthermore, the advent of single-cell technologies has opened up new avenues for biomarker analysis. Traditional bulk tissue analysis often masks cellular heterogeneity, making it challenging to identify biomarkers that are specific to certain cell types or subpopulations. Single-cell analysis techniques, such as single-cell RNA sequencing, enable researchers to examine gene expression profiles at the individual cell level, providing valuable insights into cellular diversity and disease progression.
Additionally, the field of metabolomics is gaining momentum in biomarker research. Metabolites are small molecules produced by cellular processes, and their levels can reflect the metabolic state of an organism. By analyzing metabolite profiles, researchers can uncover metabolic signatures associated with specific diseases or treatment responses, paving the way for the development of metabolite-based biomarkers.
The Potential Impact of Biomarker Analysis on Healthcare
The integration of biomarker analysis into routine clinical practice has the potential to redefine healthcare delivery. Biomarker-guided diagnostics and decision-making can enhance treatment efficacy, improve patient outcomes, and optimize healthcare resource allocation. By enabling personalized medicine, biomarker analysis has the potential to revolutionize disease management and transform the healthcare landscape.
For instance, in oncology, the identification of predictive biomarkers can help oncologists select the most effective treatment options for individual patients, minimizing unnecessary side effects and improving overall survival rates. Biomarker-based companion diagnostics can also aid in patient stratification for clinical trials, ensuring that the right patients are enrolled and increasing the chances of successful drug development.
Moreover, biomarker analysis can play a crucial role in preventive medicine. By identifying early biomarkers of disease, healthcare providers can intervene at the earliest stages, potentially preventing the development of full-blown diseases or enabling early intervention for better outcomes. This proactive approach has the potential to reduce healthcare costs and improve population health.
In conclusion, the future of biomarker analysis is filled with promise. Advances in precision medicine, artificial intelligence, multi-omic integration, single-cell technologies, and metabolomics are reshaping the field and opening up new possibilities for personalized medicine and improved healthcare outcomes. As researchers continue to uncover novel biomarkers and refine analytical techniques, the potential for biomarker analysis to revolutionize healthcare is truly exciting.
Conclusion
In conclusion, biomarker analysis represents the cutting edge of medical research, providing a deeper understanding of diseases, facilitating precise diagnoses, and guiding personalized treatment strategies. As technological advancements continue to drive the field forward, the potential impact of biomarker analysis on healthcare is unparalleled. By unraveling the complexities of biomarkers, researchers and healthcare professionals can usher in a new era of tailored medicine, shaping a future where holistic patient care thrives. Order a biomarker starter panel and discover your subhealth issues and risk factors for disease.
Lastly, if you’re interested in going deeper on health-related content, here are a few of our recent posts that you may want to read:
- Andrew Huberman is Wrong About NAD, NAD+ precursor & Longevity
- 9 Powerful Benefits of Optimizing Your NAD
- What Does Peak Performance Look Like?
- Why Optimized, Precision Medicine is the Future
Referenced Sources:
Read More