Oxidative stress is a complex biological process that plays a crucial role in both health and disease. To understand its significance, it is important first to define what oxidative stress is and explore the biochemical process of oxidation. Additionally, identifying oxidative stress markers can provide valuable insights into the body’s oxidative status.
Defining Oxidative Stress: An Overview
Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to neutralize them through antioxidant defense systems. ROS, such as free radicals, are highly reactive molecules that can cause damage to cellular structures, including DNA, proteins, and lipids.
When it comes to understanding oxidative stress, it is important to delve into the biochemical process of oxidation. Oxidation is a natural process that occurs in the body as a result of normal metabolic activities, environmental factors, and exposure to certain substances. During oxidation, molecules lose electrons, leading to the formation of ROS. This process is necessary for various physiological functions, such as energy production and cell signaling. However, excessive ROS production can tip the balance and lead to oxidative stress.
To maintain cellular balance, the body has developed an antioxidant defense mechanism system that neutralizes excessive ROS. Antioxidants, such as vitamins C and E, glutathione, and various enzymes, scavenge and neutralize free radicals, preventing them from causing damage.
Now, here is a closer look at how oxidative stress can be identified and measured. By assessing oxidative stress markers, valuable information about the body’s oxidative status can be obtained, helping in identifying potential health risks. There are several commonly used markers that researchers and healthcare professionals rely on.
Identifying Oxidative Stress Markers
Lipid peroxidation products, such as malondialdehyde (MDA), are often used as indicators of oxidative damage to lipids. Lipids are an essential component of cell membranes and play a crucial role in maintaining their integrity. When ROS attack lipids, they can cause lipid peroxidation, leading to the formation of MDA. Measuring MDA levels can provide insights into the extent of lipid damage and oxidative stress.
Another important marker of oxidative stress is DNA damage. DNA is the blueprint of life, containing the genetic information that determines our traits and functions. When ROS attack DNA, they can cause various types of damage, including oxidized DNA bases or strand breaks. Assessing these markers can help in understanding the impact of oxidative stress on the genetic material and potential consequences for cellular function.
Proteins, the workhorses of the body, are also susceptible to oxidative damage. Protein carbonyls, which are formed when proteins are attacked by ROS, reflect oxidative damage to proteins. By measuring protein carbonyl levels, researchers can gain insights into the extent of protein damage and its implications for cellular function.
Lastly, antioxidant enzyme activities can provide valuable information about the body’s defense against ROS. Superoxide dismutase (SOD) and catalase are two key antioxidant enzymes that play a crucial role in neutralizing ROS. Measuring the activity levels of these enzymes can help in assessing the body’s ability to counteract oxidative stress.
In conclusion, oxidative stress is a complex phenomenon that arises from an imbalance between ROS production and the body’s antioxidant defense mechanisms. Understanding the biochemical process of oxidation, as well as identifying and measuring oxidative stress markers, is essential for gaining insights into the impact of oxidative stress on cellular function and overall health.
The Role of Oxidative Stress Markers in Health
Maintaining cellular balance is crucial for overall health and well-being. The role of oxidative stress markers in health can be seen through their impact on various physiological processes.
Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to neutralize them with antioxidants. ROS are natural byproducts of cellular metabolism and play important roles in signaling and defense mechanisms. However, when ROS production exceeds the body’s antioxidant capacity, it can lead to oxidative damage to cellular components such as proteins, lipids, and DNA.
Maintaining Cellular Balance
When oxidative stress is controlled, it allows cells to function optimally. The delicate balance between ROS production and antioxidant defenses ensures that oxidative damage is minimized, preserving cellular integrity and promoting overall health.
One of the key markers of oxidative stress is the measurement of reactive oxygen species (ROS) levels. Various sources, including mitochondrial respiration, inflammation, and environmental factors, such as pollution and radiation, can generate ROS. Monitoring ROS levels can provide valuable insights into the cellular redox state and help identify individuals who may be at risk of oxidative damage.
In addition to ROS levels, other oxidative stress markers, such as lipid peroxidation and protein carbonylation can also be measured. Lipid peroxidation refers to the oxidative degradation of lipids, which can lead to the formation of harmful byproducts that further contribute to cellular damage. Protein carbonylation, on the other hand, is the oxidation of proteins, which can impair their structure and function.
By monitoring oxidative stress markers, healthcare professionals can gauge an individual’s oxidative status and provide tailored interventions to maintain cellular balance. These interventions may include lifestyle modifications, dietary changes, and supplementation with antioxidants to enhance the body’s defense mechanisms against oxidative stress.
The Impact on Immune Function
Oxidative stress has been shown to influence immune function. Excessive ROS production can impair immune cell function, leading to increased susceptibility to infections and compromised immune responses. Conversely, excessive antioxidant activity may suppress immune function.
The immune system1 relies on a delicate balance between pro-oxidant and antioxidant processes to mount an effective immune response. ROS plays a dual role in immune function, acting as signaling molecules to regulate immune cell activation and proliferation while also exerting antimicrobial effects. However, when ROS levels become dysregulated, it can disrupt immune cell signaling and impair their ability to fight off pathogens.
Assessing oxidative stress markers about immune function can help identify individuals at higher risk of immune-related diseases and guide appropriate interventions to restore immune balance. For example, individuals with chronic inflammatory conditions2 may benefit from antioxidant supplementation to reduce oxidative stress and support immune function.
Furthermore, oxidative stress can also contribute to the development of autoimmune diseases, where the immune system mistakenly attacks the body’s cells and tissues. By understanding the role of oxidative stress markers in immune function, researchers and healthcare professionals can gain insights into the underlying mechanisms of autoimmune diseases and develop targeted therapies.
In conclusion, oxidative stress markers play a critical role in maintaining cellular balance and influencing immune function. Monitoring these markers can provide valuable information about an individual’s oxidative status and guide interventions to promote overall health and well-being. Further research in this field is necessary to fully understand the complex interplay between oxidative stress and various physiological processes.
Oxidative Stress Markers and Disease
“Oxidative stress is a naturally occurring phenomenon behind your body’s natural aging process – but certain foods and lifestyle choices can “speed up” this process.” Dr. Meredith Warner, Orthopedic Surgeon
Oxidative stress has been implicated in the development and progression of various diseases. Medical professionals can gain insights into potential therapeutic strategies targeting oxidative stress pathways by understanding the link between oxidative stress and chronic diseases.
Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to detoxify or repair the damage. ROS are highly reactive molecules that can cause damage to cellular components, including DNA, proteins, and lipids.
Chronic diseases, such as cardiovascular disease, cancer, and diabetes, are characterized by persistent oxidative stress. ROS can contribute to the initiation and progression of these diseases by damaging cellular components and promoting inflammation.
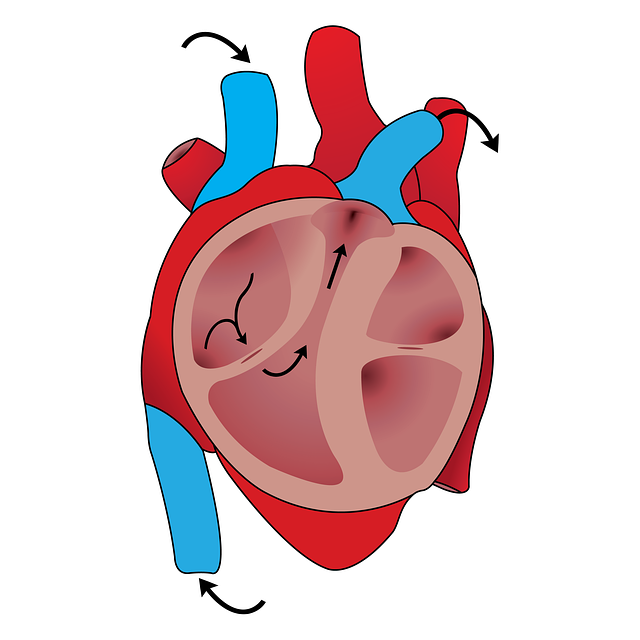
In cardiovascular disease, oxidative stress plays a key role in the development of atherosclerosis, the buildup of plaque in the arteries. ROS can oxidize low-density lipoprotein (LDL) cholesterol, leading to the formation of foam cells and the initiation of the inflammatory response. This process ultimately contributes to the narrowing of the arteries and the increased risk of heart attacks and strokes.
In cancer, oxidative stress can promote tumor growth and metastasis. ROS can induce DNA mutations and genomic instability, leading to the development of cancerous cells. Additionally, oxidative stress can activate signaling pathways that promote cell proliferation and survival, further fueling tumor growth.
In diabetes, oxidative stress is involved in the development of insulin resistance and beta-cell dysfunction. ROS can impair insulin signaling pathways and cause damage to pancreatic beta cells, leading to reduced insulin production and increased blood glucose levels.
Monitoring oxidative stress markers can aid in the early detection and prediction of chronic diseases, allowing for timely interventions and personalized treatment approaches. Biomarkers such as malondialdehyde (MDA), glutathione (GSH), and superoxide dismutase (SOD) activity can provide valuable information about the level of oxidative stress in the body.
The Link Between Oxidative Stress and Chronic Diseases
Chronic diseases, such as cardiovascular disease, cancer, and diabetes, are characterized by persistent oxidative stress. ROS can contribute to the initiation and progression of these diseases by damaging cellular components and promoting inflammation.
In cardiovascular disease, oxidative stress contributes to the development of atherosclerosis and plays a role in the formation of blood clots. ROS can activate platelets and promote their aggregation, leading to the formation of thrombi that can block blood flow and cause heart attacks or strokes.
In cancer, oxidative stress can also affect the response to chemotherapy and radiation therapy. ROS can activate cellular defense mechanisms that promote drug resistance, making cancer cells more resilient to treatment. Additionally, oxidative stress can induce DNA damage repair pathways, allowing cancer cells to survive and continue proliferating.
In diabetes, oxidative stress can further exacerbate the complications associated with the disease. ROS can contribute to the development of diabetic nephropathy, retinopathy, and neuropathy by damaging the blood vessels and nerves in these organs. This damage can lead to kidney failure, vision loss, and peripheral neuropathy, respectively.
Understanding the link between oxidative stress and chronic diseases is crucial for the development of targeted therapeutic strategies. By targeting oxidative stress pathways, researchers aim to reduce the burden of chronic diseases and improve patient outcomes.
Oxidative Stress in Neurodegenerative Diseases
Neurodegenerative diseases, including Alzheimer’s and Parkinson’s disease, have also been linked to oxidative stress. High levels of ROS can cause neuronal damage and contribute to the degenerative processes seen in these conditions.
In Alzheimer’s disease, oxidative stress plays a significant role in the accumulation of beta-amyloid plaques and neurofibrillary tangles, two hallmark features of the disease. ROS can promote the aggregation of beta-amyloid peptides, leading to the formation of plaques that disrupt neuronal communication. Additionally, oxidative stress can impair the function of mitochondria, the energy-producing organelles in cells, further contributing to neuronal dysfunction and degeneration.
In Parkinson’s disease, oxidative stress is involved in the degeneration of dopaminergic neurons in the substantia nigra, a region of the brain responsible for motor control. ROS can damage proteins involved in dopamine synthesis and transport, leading to the formation of Lewy bodies, and abnormal protein aggregates that are characteristic of the disease. Furthermore, oxidative stress can impair mitochondrial function in dopaminergic neurons, exacerbating cellular dysfunction and death.
By assessing oxidative stress markers, researchers can gain insights into disease progression and potentially develop targeted therapies to reduce oxidative stress and preserve neuronal health. Antioxidant compounds, such as vitamins C and E, have shown promise in preclinical and clinical studies for their ability to scavenge ROS and protect against neurodegeneration.
Overall, the link between oxidative stress and chronic diseases, as well as neurodegenerative diseases, highlights the importance of understanding and targeting oxidative stress pathways for the development of effective therapeutic interventions.
Measuring Oxidative Stress Markers
Accurate measurement of oxidative stress markers is essential for diagnostic purposes, research studies, and monitoring treatment efficacy. Various techniques and procedures have been developed to assess oxidative stress levels.
Diagnostic Techniques and Procedures
Common diagnostic techniques for measuring oxidative stress markers include spectrophotometry, enzyme-linked immunosorbent assays (ELISAs), and chromatography-based methods. These techniques allow for the quantification of specific markers in blood, urine, or tissue samples.
Interpreting Oxidative Stress Marker Levels
Interpreting oxidative stress marker levels requires understanding the normal range and context-specific variations. It is important to consider individual factors, such as age, gender, lifestyle, and comorbidities when assessing the significance of marker levels.
Healthcare professionals trained in oxidative stress assessment can provide valuable insights into interpreting marker levels and guide appropriate interventions based on individual needs.
Strategies to Manage Oxidative Stress
Managing oxidative stress involves a multi-faceted approach that includes lifestyle modifications and pharmacological interventions.
Lifestyle Modifications for Oxidative Stress Reduction
Adopting a healthy lifestyle is crucial for reducing oxidative stress and promoting overall well-being. This includes consuming a balanced diet rich in antioxidants, engaging in regular physical activity, managing stress levels, getting adequate sleep, and avoiding environmental toxins.
By incorporating these lifestyle modifications, individuals can enhance their antioxidant defense systems, reduce excessive ROS production, and mitigate the impact of oxidative stress on health.
Pharmacological Interventions and Therapies
In some cases, pharmacological interventions may be necessary to manage oxidative stress. Antioxidant supplements, such as vitamin C, vitamin E, and coenzyme Q10, are commonly used to augment the body’s antioxidant defenses.
Other therapeutic approaches targeting oxidative stress pathways are also being explored, including the use of targeted antioxidants, enzyme modulators, and gene therapy.
Conclusion
In conclusion, understanding the role and importance of oxidative stress markers in health and disease is crucial for improving our understanding of oxidative stress-related conditions and developing effective interventions. By defining oxidative stress, identifying markers, and exploring their impact on health and disease, healthcare professionals and researchers can better assess an individual’s oxidative status, predict disease risk, and develop personalized treatment strategies.
Furthermore, measuring oxidative stress markers and interpreting their levels accurately can aid in diagnostic processes and monitoring treatment efficacy. Implementing strategies to manage oxidative stress, such as lifestyle modifications and pharmacological interventions, can help to reduce excessive ROS production, enhance antioxidant defenses, and promote overall well-being. Order a biomarker starter panel today to get an overview of your health status.
Lastly, if you’re interested in going deeper on health-related content, here are a few of our recent posts that you may want to read:
- Understanding the Difference Between Biological Age vs. Chronological Age
- The 6 Root Causes of Aging
- Understanding Cellular Senescence: The Science of Aging & Cellular Regeneration
- Why Optimized, Precision Medicine is the Future
- Andrew Huberman is Wrong About NAD, NAD+ precursor & Longevity
Referenced Sources: