Understanding the Crucial Role of Cardiac Biomarkers in Heart Health
Cardiac biomarkers are vital in assessing heart health and diagnosing various cardiovascular conditions. These biomarkers are specific molecules or substances released into the bloodstream when the heart is damaged or under stress.
By measuring and analyzing the levels of these biomarkers, healthcare professionals can gain valuable insights into a patient’s heart function and overall cardiac health.
“Think about it: Heart disease and diabetes, which account for more deaths in the U.S. and worldwide than everything else combined, are completely preventable by making comprehensive lifestyle changes. Without drugs or surgery.” —Dean Ornish, MD
What are Cardiac Biomarkers?
Cardiac biomarkers are biological markers that can be measured in blood, urine, or other bodily fluids. These markers help healthcare providers assess the presence or severity of heart disease and monitor the effectiveness of treatments.
They provide valuable diagnostic information and are an important tool in caring for patients with cardiovascular conditions.
Defining Cardiac Biomarkers
Cardiac biomarkers are substances released into the bloodstream during heart muscle damage. They can be enzymes, proteins, hormones, or other molecules that indicate the heart’s health status. These biomarkers are often measured through blood tests and are used to diagnose heart conditions, predict prognosis, monitor treatment response, and guide therapeutic decision-making.
When heart muscle cells are injured or die, they release these biomarkers into the bloodstream. The presence and levels of these biomarkers can indicate the extent of heart damage and help healthcare providers determine the appropriate course of action.
For example, elevated levels of certain cardiac biomarkers may suggest a heart attack or heart failure, while decreasing levels may indicate that the heart is healing.
Different Types of Cardiac Biomarkers
There are several different types of cardiac biomarkers, each with its own unique characteristics and diagnostic value. Some commonly measured cardiac biomarkers include:
- Troponin: Troponin1 is a protein that regulates the contraction of heart muscle cells. Elevated levels of troponin in the blood indicate heart muscle damage, such as a heart attack.
- Creatine kinase (CK): CK is an enzyme that plays a role in energy production in cells. Increased levels of CK in the blood can indicate heart muscle damage.
- B-type natriuretic peptide (BNP): BNP is a hormone that is released by the heart in response to increased pressure and stress. Elevated levels of BNP can indicate heart failure.
- Myoglobin: Myoglobin is a protein found in heart and skeletal muscle cells. Increased levels of myoglobin in the blood can indicate muscle damage, including damage to the heart.
- C-reactive protein (CRP): CRP is a marker of inflammation in the body. Elevated levels of CRP can indicate inflammation in the heart, which may be a sign of heart disease.
- Pro-brain natriuretic peptide (proBNP): ProBNP is a precursor hormone to BNP. Elevated levels of proBNP can indicate heart failure.
- High-sensitivity cardiac troponin (hs-cTn): This is a more sensitive version of the troponin test, allowing for the detection of smaller amounts of troponin in the blood. It is used to diagnose heart attacks and assess the severity of heart muscle damage.
Each biomarker provides different information about heart health and can be used in combination to achieve a more comprehensive assessment.
For example, troponin is highly specific to heart muscle damage, while BNP is more indicative of heart failure. By measuring multiple biomarkers, healthcare providers can gather a more complete picture of a patient’s cardiovascular health and make more informed treatment decisions.
The Connection Between Cardiac Biomarkers and Heart Health
Cardiac biomarkers serve as indicators of heart health and play a crucial role in diagnosing and managing various cardiovascular conditions. These biomarkers can provide valuable information regarding heart muscle damage, inflammation, and stress. By assessing the levels of specific cardiac biomarkers, healthcare professionals can gain insights into the presence, severity, and prognosis of heart disease.
In addition to their diagnostic value, cardiac biomarkers have become an essential tool in monitoring the effectiveness of treatment strategies. By regularly measuring these biomarkers, healthcare providers can track changes in their levels over time, allowing for adjustments in medication dosages or treatment plans as needed.
How Cardiac Biomarkers Indicate Heart Health
Elevated levels of certain cardiac biomarkers, such as troponin, can indicate an increased risk of heart muscle damage or myocardial infarction (heart attack). These biomarkers are released into the bloodstream when there is injury or stress to the heart muscle. By measuring their levels, healthcare providers can determine the extent of cardiac damage and tailor appropriate treatment plans.
Another cardiac biomarker that provides valuable insights into heart health is C-reactive protein (CRP). Increased levels of CRP indicate the presence of inflammation in the body, including the blood vessels that supply the heart. Monitoring CRP levels can help healthcare professionals identify individuals at higher risk for cardiovascular diseases and implement preventive measures.
Furthermore, the measurement of cardiac troponin levels can be used not only for diagnosing heart attacks but also for risk stratification in patients with acute coronary syndromes. This allows healthcare providers to identify individuals who are at a higher risk of experiencing adverse cardiac events and provide them with more intensive monitoring and treatment.
The Role of Cardiac Biomarkers in Heart Disease
Cardiac biomarkers also play a critical role in diagnosing and managing heart diseases. For instance, elevated levels of B-type natriuretic peptide (BNP) can indicate heart failure. This biomarker is released in response to stretching of heart muscle cells, which occurs in heart failure. By monitoring BNP levels, healthcare professionals can assess the severity of heart failure and adjust treatment strategies accordingly.
In recent years, cardiac biomarkers have been increasingly used to identify individuals at risk of developing cardiovascular diseases, even before symptoms manifest. For example, high-sensitivity cardiac troponin assays can detect very low levels of troponin in the blood, allowing for early detection of myocardial injury and the initiation of preventive measures to reduce the risk of future cardiac events.
Moreover, the measurement of cardiac biomarkers such as brain natriuretic peptide (BNP) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) has proven to be valuable in the diagnosis and management of heart failure. These biomarkers are released in response to increased pressure and volume overload on the heart, providing healthcare professionals with important information about the severity of the condition and guiding treatment decisions.
In conclusion, cardiac biomarkers are essential tools in assessing heart health, diagnosing cardiovascular conditions, and managing heart diseases. By measuring the levels of specific biomarkers, healthcare professionals can gain valuable insights into the presence, severity, and prognosis of heart disease, allowing for personalized treatment plans and improved patient outcomes.
The Importance of Monitoring Cardiac Biomarkers
Regular monitoring of cardiac biomarkers is essential for individuals at risk of heart disease or those already diagnosed with cardiovascular conditions. It helps healthcare providers assess the effectiveness of treatments, measure disease progression, and determine the need for therapeutic interventions.
Regular Testing for Cardiac Biomarkers
Patients with known heart conditions often undergo regular testing to monitor their cardiac biomarker levels. These tests can help identify early signs of worsening heart function or detect potential complications. Healthcare professionals can adjust medications, initiate preventive measures, or recommend further diagnostic tests by detecting changes in biomarker levels.
In addition to troponin, other cardiac biomarkers that may be monitored include B-type natriuretic peptide (BNP) and creatine kinase-MB (CK-MB). BNP levels can indicate heart failure, while CK-MB levels can indicate damage to the heart muscle.
Regular testing for cardiac biomarkers is especially important for individuals with a history of heart disease or those who have recently undergone cardiac procedures, such as angioplasty2 or bypass surgery. These individuals are at a higher risk of complications, and monitoring their biomarker levels can help detect any issues early on.
Interpreting Cardiac Biomarker Levels
Interpreting cardiac biomarker levels requires a comprehensive understanding of the specific biomarkers being measured. Healthcare providers consider factors such as baseline levels, reference ranges, timing of measurements, and the clinical context to interpret the results accurately. Trends in biomarker levels over time are vital in assessing disease progression and treatment response.
For example, if a patient’s troponin levels have been steadily increasing over several tests, it may indicate ongoing damage to the heart muscle. This information can prompt healthcare providers to adjust medications, recommend lifestyle changes, or consider more aggressive treatment options.
It’s important to note that cardiac biomarker levels can also be influenced by factors other than heart disease. For instance, certain medications, kidney problems, or skeletal muscle injuries can affect the accuracy of the results. Therefore, healthcare providers must take these factors into account when interpreting biomarker levels.
In conclusion, regular monitoring of cardiac biomarkers is crucial for individuals at risk of heart disease or those already diagnosed with cardiovascular conditions. By tracking these biomarkers, healthcare professionals can gain valuable insights into the heart’s health and make informed decisions about patient care.
The Future of Cardiac Biomarkers in Heart Health
Ongoing research and advancements in technology hold promising potential for the future of cardiac biomarkers. Researchers continually investigate new biomarkers and refine existing tests to improve diagnosis, risk assessment, and treatment strategies for heart diseases.
Advances in Cardiac Biomarker Research
Research in the field of cardiac biomarkers aims to identify novel markers that can provide more accurate and specific information about cardiac health. The development of high-sensitivity cardiac troponin assays has greatly improved the precision and sensitivity of detecting heart muscle damage. In the future, advancements in genetic testing and proteomics may lead to the discovery of additional biomarkers that can further enhance heart disease diagnosis and management.
Potential New Uses for Cardiac Biomarkers in Heart Health Care
Cardiac biomarkers are not limited to diagnosing and managing existing heart conditions. They also have the potential to be used in preventive healthcare. By identifying individuals at high risk of developing heart disease based on their biomarker profiles, healthcare providers can intervene early with lifestyle modifications, medications, or other preventive measures to reduce the risk of cardiovascular events.
Conclusion
In conclusion, cardiac biomarkers are critical tools in evaluating heart health and diagnosing cardiovascular conditions. The measurement and analysis of these biomarkers provide valuable insights into heart function, disease presence, and treatment response. As research continues to advance, cardiac biomarkers will undoubtedly play an increasingly important role in promoting heart health and improving patient outcomes. Click here to order a biomarker test to check your heart health.
Lastly, if you’re interested in going deeper on health-related content, here are a few of our recent posts that you may want to read:
- Why Optimized, Precision Medicine is the Future
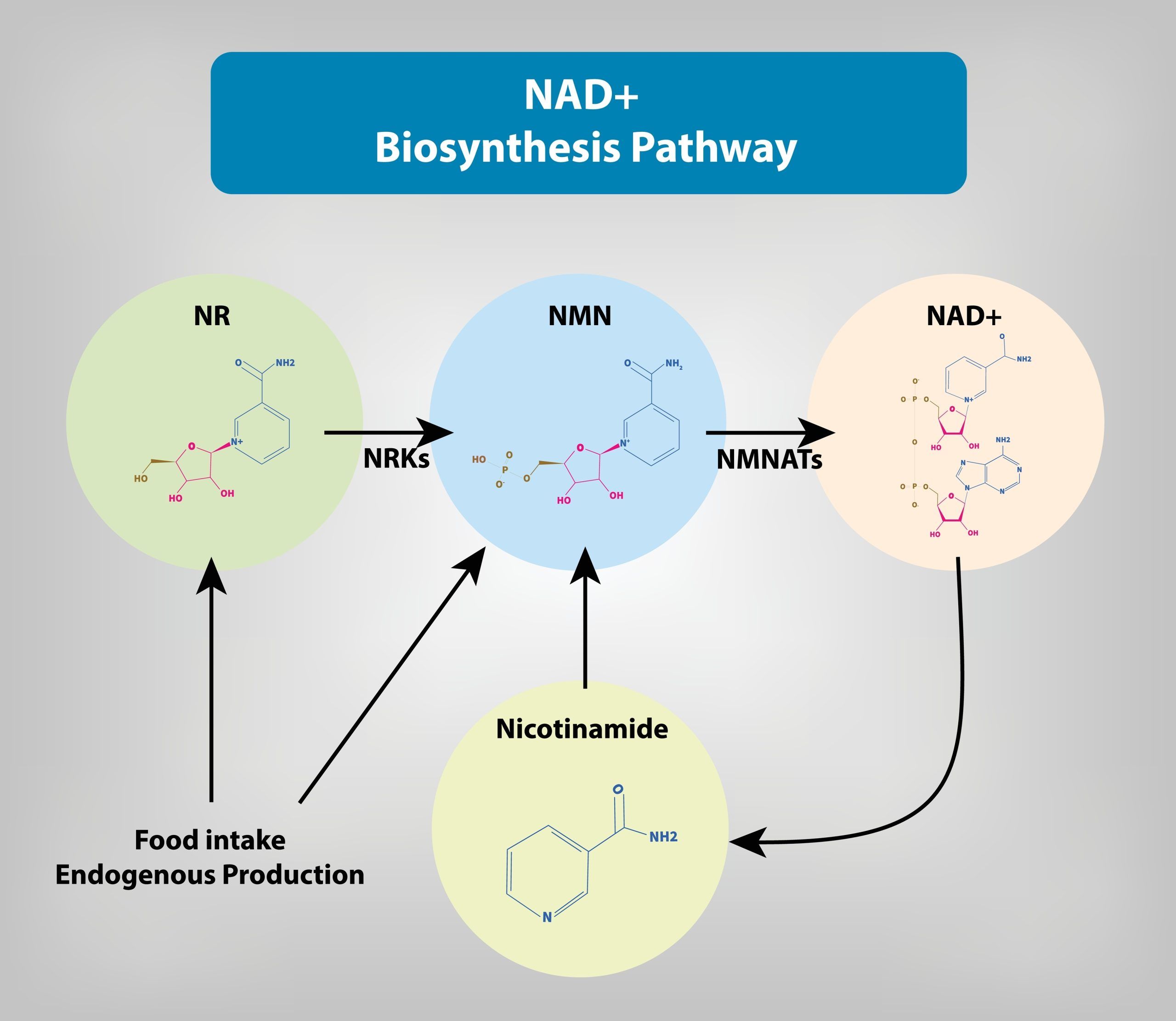
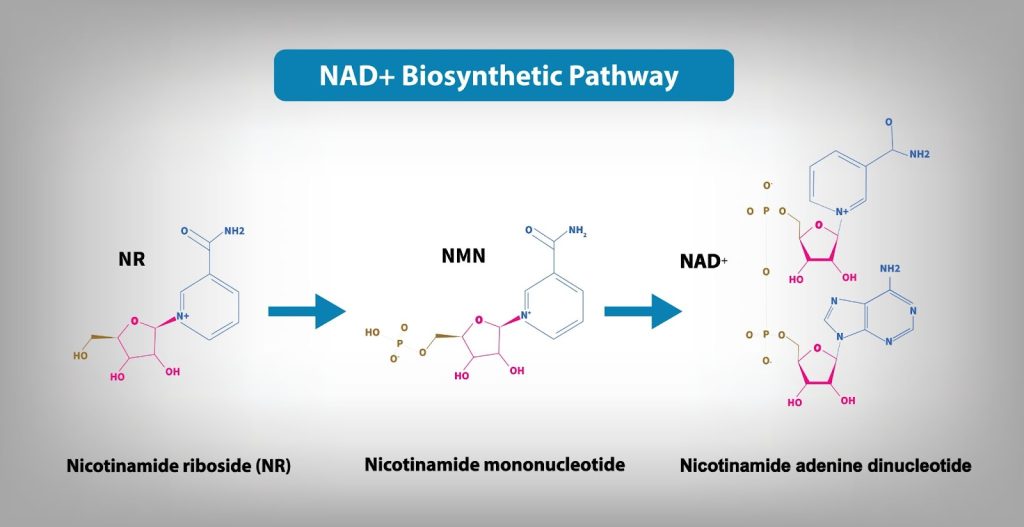
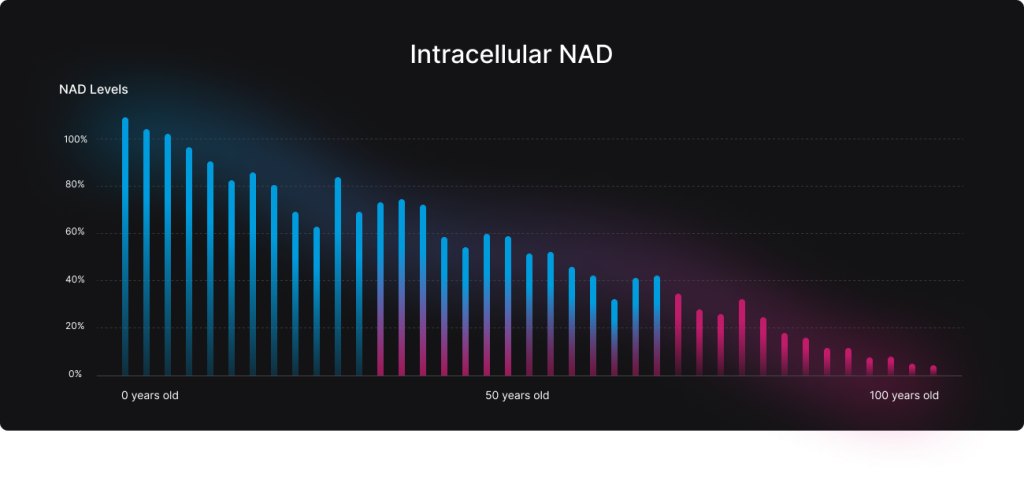
- 9 Powerful Benefits of Optimizing Your NAD
- What Does Peak Performance Look Like?
- Andrew Huberman is Wrong About NAD, NAd+ precursor & Longevity